






Cancer Survivorship and Chemotherapy-Induced Peripheral Neuropathy
 How would it be... if simple use of hands-on techniques by a loved one could reduce, eliminate or prevent peripheral neuropathy in cancer survivors undergoing chemotherapy?
How would it be... if simple use of hands-on techniques by a loved one could reduce, eliminate or prevent peripheral neuropathy in cancer survivors undergoing chemotherapy?
This project is developing an instructional mobile app to provide expert guidance in simple massage techniques to address and alleviate a common long-term adverse impact of chemotherapy for which there has been no conventional medical treatment. We are working with a team of leading oncology massage therapists who have pioneered and refined an effective protocol through work with thousands of chemotherapy patients. The goal is to develop a caregiver education mobile app for instruction at home, so caregivers can easily apply it to their loved ones who have or are at risk of developing CIPN. This follows our earlier work developing the award-winning Touch, Caring and Cancer program, now being used in cancer support and palliative care programs across the US and in several other countries.
Who is conducting the project?
- The organization leading the study is Collinge and Associates, Inc., an independent research organization funded by the National Institutes of Health. This project involves a collaboration with Mayo Clinic-Florida for conducting a randomized controlled clinical trial.
- The Principal Investigators are William Collinge, PhD and Cindy Tofthagen, PhD, APRN, AOCNP, FAANP, FAAN of Mayo Clinic College of Medicine and Science
- The project is sponsored by the National Cancer Institute, grant #R44CA268678
- Collaborators include Healwell, Mayo Clinic, and Trifoia Digital Learning
What's next?
This Phase II project is underway from June, 2024-May, 2026. After completing development of the mobile app we will be conducting a randomized controlled clinical trial with 150 cancer survivors and their care partners through a collaboration with Mayo Clinic-Florida. Watch this space for news of the project and its outcomes.
Integrative Palliative Care: CE/CME Program
 How would it be... if health professionals working in palliative and end-of-life care could confidently make evidence-informed recommendations on complementary therapies to reduce suffering and improve quality of life?
How would it be... if health professionals working in palliative and end-of-life care could confidently make evidence-informed recommendations on complementary therapies to reduce suffering and improve quality of life?
Palliative care represents one of the most rapidly expanding sectors of health care. Integrative therapies have been shown to offer comfort, reduce suffering, and improve the quality of life in palliative care patients. The evidence is growing, and an increasing number of patients seek such therapies. There is a need for CE/CME opportunities to help palliative care personnel make evidence-informed care planning decisions concerning the use of integrative therapies.
A new online CE/CME program is now available to multidisciplinary palliative care professionals on the evidence-informed use of integrative therapies in palliative care populations. The 9-module program was developed and evaluated with research funding from the National Cancer Institute.
Two formats are available for taking the program. A self-paced "fasttrack" format is for those who don't need CE/CME credits. Learn at your own pace, and stream all content without quizzes or tests. A CE/CME format is available for those who would like to receive 9 CE/CME credits for the program granted by the National Hospice and Palliative Care Organization (NHPCO), a Jointly Accredited Provider of Interprofessional Continuing Education for the healthcare team.
A Phase II randomized controlled trial with 170 physicians, nurses, social workers, chaplains, and other palliative care professionals found the program led to significant improvements in their confidence in understanding the modalities, as well as increased practice behaviors that encourage integrative care such as communicating with patients, family members and colleagues about integrative therapies, recommending their use, and promoting culture change in their organizations to encourage integrative care.
See the full study published in the journal Global Advances in Integrative Medicine and Health. This is the first online continuing education program with documented impact on practice behaviors that promote integrative care.
The Principal Investigators of the project, William Collinge, PhD and Leila Kozak, PhD, have created the Integrative Palliative Care Institute as a new educational organization that hosts and disseminates the program. A distinguished faculty of national experts in palliative care participate in delivery of the course content. Topics covered include:
- Acupuncture and related approaches
- Massage and bodywork approaches
- Biofield therapies (Reiki, Healing Touch, etc.)
- Aromatherapy
- Expressive arts therapies
- Mind/body and contemplative approaches
- Movement approaches
- Transforming the culture of palliative care
Who is the program for?
Physicians, physician assistants, nurse practitioners, nurses, social workers, psychologists, counselors, pharmacists, administrators, chaplains, and others working in palliative care.
CLICK HERE FOR FULL DETAILS AND ACCESS TO THE PROGRAM.
Collaborators
- The organization conducting the study was Collinge and Associates, Inc., an independent research organization funded by the National Institutes of Health
- Sponsored by National Cancer Institute grant #R44 CA210723
- Principal Investigators: William Collinge, PhD and Leila Kozak, PhD
- National Hospice and Palliative Care Organization (NHPCO)
- Trifoia Digital Learning, Eugene, OR
African American Family Caregivers and End-of-Life Care in Dementia
 How would it be... if underserved African American families who have a loved one with dementia were well-prepared to deal with end-of-life treatment decisions?
How would it be... if underserved African American families who have a loved one with dementia were well-prepared to deal with end-of-life treatment decisions?
ACTPlan® (Advance Care Treatment Planning) is a culturally-tailored educational program for African American family caregivers with decisional responsibility for loved ones with dementia. The program was created by Gloria Bonner, PhD, RN, FAAN, of Bonner-Platt & Associates, LLC. Dr. Bonner’s previous research with ACTPlan® found significant improvements in caregiver knowledge and self-efficacy in advance care treatment planning and decision-making.
From 2019-23, with funding from the National Institute on Aging, Collinge and Associates, Inc. and Bonner-Platt & Associates, LLC collaborated to develop and evaluate a new online, multimedia version of ACTPlan® that could facilitate wide dissemination and help reduce disparities in the quality of dementia care and support in underserved African American communities. A randomized controlled trial found the online version achieved outcomes comparable to those of the original in-person program. Publication of the new study results is forthcoming.
The online version of ACTPlan® is now available both individually and through faith-based and secular organizations who share the mission of helping reduce disparities in dementia care and caregiver support. For details and access visit www.ACTPlan.org.
Funding: National Institute on Aging grant #R44AG065095.
Related article: Bonner GJ, Freels S, Ferrans C, Steffen A, Suarez ML, Dancy BL, Watkins YJ, Collinge W, Hart AS, Aggarwal NT, Wilkie DJ. Advance Care Planning for African American Caregivers of Relatives With Dementias: Cluster Randomized Controlled Trial. Am J Hosp Palliat Care. 2020 Apr 20;:1049909120916127. doi: 10.1177/1049909120916127. PubMed PMID: 32308012.
Collaborators:
- William Collinge, Ph.D., Principal Investigator, Collinge and Associates, Inc., Eugene, OR
- Gloria J Bonner, PhD, RN, FAAN, Principal Investigator, Originator of the ACTPlan Program, Bonner-Platt & Associates, LLC, Chicago, IL
- Yashika Watkins, PhD, MPH, Chicago State University
- Neelum Aggarwal, MD, FAMWA, Rush University Medical Center
- Alysha Hart, PhD, APRN, NP-C, University of Illinois-Chicago
- Geraldine Peacock, RN, MBA, PhD, Apostolic Faith Church, Chicago
- Sally Freels, PhD, University of Illinois-Chicago
- Osei Bekoe, MPH, University of Illinois Cancer Center
- Trifoia Digital Learning, Eugene, OR
Mission Reconnect
 How would it be... if Veterans and their intimate partners could help each other heal from separation and trauma by deepening their capacity for compassion, relaxation, and mutual support? This project took place online and was funded by the National Institute of Mental Health, NIH.
How would it be... if Veterans and their intimate partners could help each other heal from separation and trauma by deepening their capacity for compassion, relaxation, and mutual support? This project took place online and was funded by the National Institute of Mental Health, NIH.
Watch a preview of the program below, and learn more at MissionReconnect.com.
Mission Reconnect is an evidence-based program of mind- and body-based therapies for use by Veterans and their Partners to support physical, mental, and relationship health. The program is delivered completely online via the Mission Reconnect website and mobile app. Winner of the Excellence in Research on Military and Veteran Families Award for 2017. Learn more and watch the introductory video at MissionReconnect.com.
Development and evaluation were sponsored by the US National Institute of Mental Health from 2010-2015. Phase I involved a feasibility study with 43 Oregon and Vermont National Guard post-9/11 Veterans and their Partners. Results were published in the journal Military Medicine, December 2012 (read the article here).
Phase II was a four-arm randomized controlled trial with 160 post-9/11 Veteran/Partner dyads from all military branches in San Diego, Dallas, Fayetteville NC, and New York. Results were published in the Journal of Medical Internet Research, September 2016 (read the article here).
Benefits for Veterans and their partners: Mission Reconnect was found to lead to significant improvements in measures of PTSD, anxiety, depression, sleep quality, perceived stress, resilience, self-compassion, pain, tension, and irritability in both Veterans and their partners.
Access: Lifetime access is available for a one-time cost of $20 and includes a free partner account for a spouse or loved one. Organizational sponsorships are also available to give free access to Veterans and their loved ones.
Slide presentation on the Mission Reconnect research: Veterans and their partners: reducing PTSD with home-based intervention. Presented at the 23rd Annual Combat Stress Conference in San Diego, April 29, 2016.
This project was funded by NIMH grant #1R43/44MH088063 to Collinge and Associates, Inc.
Ongoing research. The Veterans Health Administration is currently conducting a four-year study of the effects of Mission Reconnect in Veterans experiencing chronic pain and PTSD. More info.
PROJECT COLLABORATORS
- William Collinge, Ph.D., Principal Investigator, Collinge and Associates, Inc., Eugene, OR
- Janet Kahn, Ph.D., Principal Investigator, Peace Village Projects, Inc., and University of Vermont College of Medicine, Burlington, VT
- David Kearney, MD, Director, Mindfulness-Based Stress Reduction, VA Puget Sound Health Care System, Seattle, WA
- Jerry Wesch, Ph.D., Director, Warrior Combat Stress Reset Program, Darnell Medical Center, Fort Hood, TX
- Wayne Jonas, MD, LTC (US Army, Ret.), President and CEO, Samueli Institute, Alexandria, VA; Georgetown University Medical School, Washington
- Iraq and Afghanistan Veterans of America, New York, and Washington
- Cross Current Communications, Portsmouth, NH
- InterVision Media, Eugene, OR
AwareHealth Online Program

How would it be... if sufferers of chronic health conditions could use artificial intelligence and personal health informatics to discover how to reduce their symptoms? This project was conducted online and funded by the National Institute for Arthritis, Musculoskeletal and Skin Diseases, NIH.
The AwareHealth program can be individually tailored to be a personalized intervention for help with such diverse conditions as ME/CFS, fibromyalgia, long-COVID and cancer, as well as mental health conditions such as anxiety, depression and trauma. Learn more at AwareHealth.org.
Abstract
 Background: Personal health informatics has potential to help patients discover personalized health management strategies that influence outcomes. Fibromyalgia (FM) is a complex chronic illness requiring individualized strategies that may be informed by analysis of personal health informatics data. An online health diary program with dynamic feedback was developed to assist FM patients in identifying symptom management strategies that predict their personal outcomes, and found reduced symptom levels associated with program utilization.
Background: Personal health informatics has potential to help patients discover personalized health management strategies that influence outcomes. Fibromyalgia (FM) is a complex chronic illness requiring individualized strategies that may be informed by analysis of personal health informatics data. An online health diary program with dynamic feedback was developed to assist FM patients in identifying symptom management strategies that predict their personal outcomes, and found reduced symptom levels associated with program utilization.
Objective: The objective of this study was to determine longitudinal associations between program utilization and functional impact of FM as measured by scores on a standardized assessment instrument, the Fibromyalgia Impact Questionnaire (FIQ).
Methods: Subjects were self-identified as diagnosed with FM and recruited via online FM advocacy websites. Subjects used an online health diary program (“SMARTLog”) reporting symptom ratings, behaviors and management strategies, and providing individualized recommendations (“SMARTProfile”) based on single subject analysis of the individual’s personal accumulated data over time. Indices of program utilization comprised cumulative numbers of SMARTLogs completed and SMARTProfiles received. Subjects included in this analysis met a priori criteria of sufficient program utilization to generate SMARTProfiles; i.e., 22+ SMARTLogs completed. Users completed the FIQ at baseline and again each subsequent month of program use as follow-up data for analysis. Kendall's tau-b (τ), a nonparametric statistic that measures both the strength and direction of an ordinal association between two repeated measured variables, was computed between all available FIQ scores and both indices of program utilization for each subject at the time of each completed FIQ.
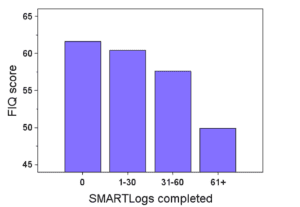 Results: 76 users met selection criteria. Mean baseline FIQ score was 61.6 (SD=14.7), and 342 FIQ scores were used in longitudinal analysis via Kendall's τ. Statistically significant inverse associations were found over time between FIQ scores and (1) cumulative number of SMARTLogs completed (τ = -0.135, P<.0003) and cumulative number of SMARTProfiles received (τ = -0.133, P<.0009). Users who completed 61 or more SMARTLogs had mean follow-up scores of 49.9 (33.3% of the sample), an 18.9% drop in FM impact. Users who generated 11 or more new SMARTProfiles had mean follow-up scores of 51.8 (30% of the sample), a 15.9% drop.
Results: 76 users met selection criteria. Mean baseline FIQ score was 61.6 (SD=14.7), and 342 FIQ scores were used in longitudinal analysis via Kendall's τ. Statistically significant inverse associations were found over time between FIQ scores and (1) cumulative number of SMARTLogs completed (τ = -0.135, P<.0003) and cumulative number of SMARTProfiles received (τ = -0.133, P<.0009). Users who completed 61 or more SMARTLogs had mean follow-up scores of 49.9 (33.3% of the sample), an 18.9% drop in FM impact. Users who generated 11 or more new SMARTProfiles had mean follow-up scores of 51.8 (30% of the sample), a 15.9% drop.
Conclusions: Significant inverse associations were found between FIQ scores and both indices of program utilization, with FIQ score declining as utilization increased. Based on established criteria for rating FM severity, the top third of users in terms of utilization had clinically significant reductions from “severe” to “moderate” FM impact. These findings underscore the value of self-management interventions with low burden, high usability and high perceived relevance to the user. Clinical Trial: ClinicalTrials.gov NCT02515552
William Collinge, Paul Yarnold, Rob Soltysik. Fibromyalgia Symptom Reduction by Online Behavioral Self-monitoring, Longitudinal Single Subject Analysis and Automated Delivery of Individualized Guidance. N Am J Med Sci. 2013 Sep;5(9):546-53.
Abstract
Background: Fibromyalgia (FM) is a complex chronic pain condition that is difficult to treat. The prevailing approach is an integration of pharmacological, psycho-educational, and behavioral strategies. Information technology offers great potential for FM sufferers to systemically monitor symptoms as well as potential impacts of various management strategies.
Aims: This study aimed to evaluate effects of a web-based, self-monitoring and symptom management system (SMARTLog) that analyzes personal self-monitoring data and delivers data-based feedback over time.
Materials and Methods: Subjects were self-referred, anonymous, and recruited via publicity on FM advocacy websites. Standardized instruments assessed health status, self-efficacy, and locus of control at baseline and monthly during participation. Subjects were encouraged to complete the SMARTLog several times weekly. Within-subject, univariate, and multivariate analyses were used to derive classification trees for each user associating specific behavior variables with symptom levels over time.
Results: Moderate use (3 times weekly x 3 months) increased likelihood of clinically significant improvements in pain, memory, gastrointestinal problems, depression, fatigue, and concentration; heavy use (4.5 times weekly x five months) produced the above plus improvement in stiffness and sleep difficulties.
Conclusions: Individualized, web-based behavioral self-monitoring with personally-tailored feedback can enable FM sufferers to significantly reduce symptom levels over time.
Collaborators:
- William Collinge, Ph.D., Principal Investigator, Collinge and Associates, Inc., Eugene, OR
- Paul Yarnold, PhD, Northwestern University Feinberg School of Medicine
- Rob Soltysik, MS, Optimal Data Analysis, LLC, Severn, MD
- Fred Friedberg, PhD, State Univ. of New York Stonybrook, Dept of Psychiatry
- Don Goldenberg, MD, Newton-Wellesley Hospital and Tufts Medical School
Touch, Caring and Cancer
 How would it be... if care partners could easily provide comfort to cancer patients that reduced their symptoms, made caregiving more satisfying, and improved the quality of their relationship? This study took place with families from several cancer treatment organizations in Boston, MA and Portland, OR, and was sponsored by the National Cancer Institute, NIH.
How would it be... if care partners could easily provide comfort to cancer patients that reduced their symptoms, made caregiving more satisfying, and improved the quality of their relationship? This study took place with families from several cancer treatment organizations in Boston, MA and Portland, OR, and was sponsored by the National Cancer Institute, NIH.
Winner of two Telly Awards, and featured on NCI's Research-Tested Intervention Programs (RTIPS) website. Watch a preview of the program below and learn more here.
William Collinge, Janet Kahn, Tracy Walton, Leila Kozak, Susan Bauer-Wu, Kenneth Fletcher, Paul Yarnold, Rob Soltysik, Touch, Caring, and Cancer: randomized controlled trial of a multimedia caregiver education program. Supportive Care in Cancer. 2013 May;21(5):1405-14.
Abstract
PURPOSE: A randomized controlled trial was conducted to evaluate outcomes of a multimedia instructional program for family caregivers in simple touch-based techniques to provide comfort to cancer patients at home.
METHODS: A multilingual 78-min DVD and 66-page manual were produced for home-based instruction. Content addresses attitudes and communication about touch in cancer, psychological preparation for giving and receiving touch, safety precautions, massage techniques for comfort and relaxation, acupressure for specific cancer-related symptoms, and practice in the home setting. Materials were produced in English, Spanish, and Chinese versions. A community-based multi-ethnic sample of 97 adult patient/caregiver dyads was randomized to experimental (massage) or attention control (reading) groups for 4 weeks. Massage dyads received the program and instructions to practice at least three times per week, while control caregivers read to their patients for the same frequency. Self-report instruments assessed change in symptom severity, quality of life, perceived stress, and caregiver attitudes.
RESULTS: Significant reductions in all symptoms occurred for patients after both activities: 12-28 % reductions after reading vs. 29-44 % after massage. Massage caregivers showed significant gains in confidence, comfort, and self-efficacy using touch and massage as forms of caregiving.
CONCLUSIONS: Multimedia instruction in touch and massage methods may offer family members a viable means of enhancing self-efficacy and satisfaction in caregiving while decreasing patient pain, depression, and other symptoms. Family members may be able to learn and apply safe and simple methods that increase patient comfort and reduce distress.
*PROGRAM AVAILABILITY: The Touch, Caring and Cancer Program is available as streaming media in English, Spanish, Mandarin, Cantonese and Vietnamese at www.IntegrativePalliativeCare.org.
The Elder Healer Project
 How would it be... if the elders among us held untapped healing abilities that could be discovered and developed to the benefit of us all – at the same time making their own lives more meaningful and fulfilling? This study took place in Boston and was funded by the National Institute on Aging, NIH.
How would it be... if the elders among us held untapped healing abilities that could be discovered and developed to the benefit of us all – at the same time making their own lives more meaningful and fulfilling? This study took place in Boston and was funded by the National Institute on Aging, NIH.
The study conducted experiential workshops with sixty elders. Subjects had significant increases in perceived self-efficacy and use of touch in interpersonal caregiving, evidence of significant associations between use of touch and mental health and well-being, and evidence of the positive impact of the training on personal development.
This project suggests that elders can easily learn techniques that contribute to public health by benefiting elders themselves as well as their families, friends, and others in their natural social environment whom they will serve with their new skills.
Collaborator:
- Diane Wind Wardell PhD, RN, WHNP,AHN-BC, CHTP/I Professor of Nursing at University of Texas Health Science Center Houston, School of Nursing
Integrative Therapies in Community Mental Health
How would it be... if simple touch and energy therapies have psychotherapeutic effects, and could magnify the effectiveness of traditional mental health services? This study took place at Counseling Services, Inc., a community mental health center in Saco, ME.
William Collinge, Roberta Wentworth, Sherry Sabo. Integrating complementary therapies into community mental health practice: an exploration. J Altern Complement Med. 2005 Jun;11(3):569-74.
 ABSTRACT
ABSTRACT
OBJECTIVES: To (1) describe the integration of massage and energy-based therapies with psychotherapy in a community mental health center, (2) to present qualitative feedback on the service, and (3) to present pilot data from a sample of long-term clients with persistent mental health concerns. DESIGN: A noncontrolled pilot study was conducted using interview data before and self-report instruments after completing a brief program of complementary therapy accompanying ongoing psychotherapy. SETTINGS/LOCATION: The program took place at a comprehensive community mental health center in southern Maine and in the private offices of massage therapists and energy healing practitioners who contracted with the program. SUBJECTS: Subjects were 20 women and 5 men, with a mean age of 42 years and a mean history of 7.4 years of mental health treatment. All had histories that included trauma, 10 of which involved sexual abuse. The Diagnostic and Statistical Manual of Mental Disorders-IV Axis I diagnoses were PTSD (10), major depression (nine), anxiety disorder (three), and dual diagnosis (three). INTERVENTIONS: Clients receiving ongoing psychotherapy were assigned to one modality of complementary therapy based on clinical judgment, availability of practitioners, and client interest. Modalities used were massage, acupuncture, Reiki, and Healing Touch. The mean number of sessions was five. OUTCOME MEASURES: Clients completed an investigator-generated instrument with Likert-scaled ratings of satisfaction and perceived changes in four dimensions of trauma recovery: perceived interpersonal safety, interpersonal boundary setting, bodily sensation, and bodily shame. RESULTS: Clients reported high levels of satisfaction with the service and significant levels of perceived (self-rated) change on each outcome measure. Qualitative results included enhanced psychotherapeutic outcomes reported by mental health clinicians. CONCLUSIONS: The integration of complementary therapies into community mental health practice may hold the promise of enhancing mental health outcomes and improving the quality of life for long-term users of mental health services.
Mindfulness and Qigong in Chronic Fatigue Syndrome
How would it be... if the regular practice of mindfulness meditation and qigong could improve the long-term course of CFS? This study took place at the Flowing River Institute in San Francisco, and was funded by the Stupski Foundation.
William Collinge, Paul Yarnold, Ellen Raskin. Use of Mind/Body Self-Healing Practice Predicts Positive Health Transition in Chronic Fatigue Syndrome: A Controlled Study. Subtle Energies & Energy Medicine, 1998;9(3):171-90.
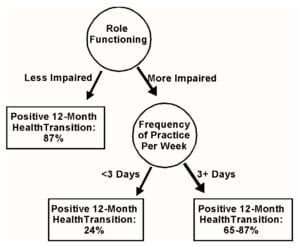
 Abstract. Seventy subjects diagnosed with chronic fatigue syndrome were randomized to a control group (N = 33) or a treatment group (N = 37). All continued usual medical care. Treatment subjects were assigned to a 9 week, 2-hours-per-week group program teaching mindfulness meditation and medical qigong practices. The outcome variable was 12-month health transition at one-year follow-up, as defined by the SF36 12-month Health Transition score. The data yielded a classification tree with a 90% overall accuracy rate in classifying subjects as "improvers" or non-improvers" (effect strength 80.5, experimentwise p < .05), based on SF36 Role FunctioningPhysical score at follow-up and frequency of mind/body self-healing practice. Subjects in the highest quartile of Role Functioning-Physical improved regardless of practice. For the remaining 75%, those practicing three or more days per week at follow-up were 2.7 times more likely to report positive 12-month Health Transition than those practicing less.
Abstract. Seventy subjects diagnosed with chronic fatigue syndrome were randomized to a control group (N = 33) or a treatment group (N = 37). All continued usual medical care. Treatment subjects were assigned to a 9 week, 2-hours-per-week group program teaching mindfulness meditation and medical qigong practices. The outcome variable was 12-month health transition at one-year follow-up, as defined by the SF36 12-month Health Transition score. The data yielded a classification tree with a 90% overall accuracy rate in classifying subjects as "improvers" or non-improvers" (effect strength 80.5, experimentwise p < .05), based on SF36 Role FunctioningPhysical score at follow-up and frequency of mind/body self-healing practice. Subjects in the highest quartile of Role Functioning-Physical improved regardless of practice. For the remaining 75%, those practicing three or more days per week at follow-up were 2.7 times more likely to report positive 12-month Health Transition than those practicing less.
Breathwork and Immunity
How would it be... if a simple practice of breathing with evocative music and guided imagery could stimulate immune functioning in people with cancer and other illnesses? This project evaluated effects of a transformational breathwork process used with cancer patients and their partners in an integrative therapies program. The study took place at the Cancer Support and Education Center, Menlo Park, CA, and was funded by the Strom Family Foundation.
William Collinge and Paul Yarnold. Transformational Breath Work in Medical Illness: An Exploration and Evidence of Immuno-Enhancement. Subtle Energies & Energy Medicine, 2001,12(2):61-78
ABSTRACT The term “transformational breathwork” commonly refers to techniques that use the breath for inducing altered states of consciousness to promote healing on any level. This paper describes common elements of transformational breathwork and rationale for its use in medical illness. It then describes the use of one form, Evocative Breath Therapy (EBT), within a group mind/body medicine program. The technique employs an hour-long, four-stage process of focused awareness on the breath accompanied by guided imagery and evocative music. It is designed to induce an altered state of consciousness that promotes expanded self-awareness, self-acceptance, self-compassion, a sense of inner peace, and release of emotional and physical tension. A pilot study was conducted to determine the impact of EBT on one indicator of immune function, salivary immunoglobulin A (S-IgA). A heterogeneous sample of forty-five adults (21 cancer patients, 22 healthy others, 2 with other illnesses) contributed saliva samples before and immediately after the experience. A 46.3% increase in S-IgA was found (p=.0123, paired-differences t-test). There were no significant differences between cancer patients and others. Effect strength was moderate, .278. Leave-one-out analysis found the effect strength to decrease only marginally, suggesting the results are likely generalizable to independent random samples. Issues in the use of transformational breathwork in clinical programs and implications for further research are discussed.
The term “transformational breathwork” commonly refers to techniques that use the breath for inducing altered states of consciousness to promote healing on any level. This paper describes common elements of transformational breathwork and rationale for its use in medical illness. It then describes the use of one form, Evocative Breath Therapy (EBT), within a group mind/body medicine program. The technique employs an hour-long, four-stage process of focused awareness on the breath accompanied by guided imagery and evocative music. It is designed to induce an altered state of consciousness that promotes expanded self-awareness, self-acceptance, self-compassion, a sense of inner peace, and release of emotional and physical tension. A pilot study was conducted to determine the impact of EBT on one indicator of immune function, salivary immunoglobulin A (S-IgA). A heterogeneous sample of forty-five adults (21 cancer patients, 22 healthy others, 2 with other illnesses) contributed saliva samples before and immediately after the experience. A 46.3% increase in S-IgA was found (p=.0123, paired-differences t-test). There were no significant differences between cancer patients and others. Effect strength was moderate, .278. Leave-one-out analysis found the effect strength to decrease only marginally, suggesting the results are likely generalizable to independent random samples. Issues in the use of transformational breathwork in clinical programs and implications for further research are discussed.